Hypertension, often referred to as the “silent killer,” is a chronic condition that affects millions worldwide, significantly increasing the risk of cardiovascular diseases, stroke, and organ failure. Many individuals with high blood pressure experience no symptoms for years, allowing the condition to cause progressive damage before detection. Left uncontrolled, hypertension can lead to severe complications such as heart attacks, aneurysms, kidney dysfunction, and cognitive decline. The condition is influenced by various factors, including genetics, lifestyle choices, obesity, and underlying medical conditions such as diabetes and kidney disease. Since hypertension develops gradually, regular monitoring and early assessment of organ damage are essential for effective management and prevention of complications.
Although hypertension is primarily diagnosed using blood pressure measurements, imaging tests play a crucial role in evaluating the damage caused to vital organs. One of the most commonly used imaging techniques is echocardiography, which helps assess the effects of prolonged high blood pressure on the heart. Chronic hypertension forces the heart to pump harder, leading to left ventricular hypertrophy (LVH)—a thickening of the heart muscle that increases the risk of heart failure. Echocardiography provides real-time visualization of heart chamber sizes, wall thickness, and overall cardiac function. In cases of severe or long-standing hypertension, cardiac MRI may be performed to provide a more detailed assessment of myocardial fibrosis (scarring of heart tissue) and ventricular remodeling.
In addition to cardiac imaging, carotid ultrasound is frequently used to assess vascular health in hypertensive patients. High blood pressure contributes to the formation of atherosclerotic plaques—fatty deposits that accumulate in the carotid arteries and increase the risk of strokes. Carotid ultrasound uses Doppler imaging to evaluate blood flow patterns and detect narrowing (stenosis) of the arteries. Detecting early vascular damage allows doctors to recommend preventive measures, such as cholesterol-lowering medications and lifestyle changes, to reduce stroke risk. Computed tomography angiography (CTA) or magnetic resonance angiography (MRA) may also be used in high-risk patients to obtain a more detailed view of the blood vessels in the brain and neck.
Hypertension is also a leading cause of chronic kidney disease (CKD), making renal imaging essential for patients with persistently high blood pressure. Renal Doppler ultrasound is the first-line imaging test to evaluate renal artery stenosis, a condition where narrowing of the arteries supplying the kidneys leads to secondary hypertension. Reduced kidney perfusion can cause an increase in blood pressure, further damaging kidney function. In cases where ultrasound results are inconclusive, CT or MRI angiography is performed to obtain high-resolution images of the renal arteries and surrounding structures. Kidney damage due to hypertension is often irreversible, making early detection and intervention critical in preventing the progression to end-stage renal disease.
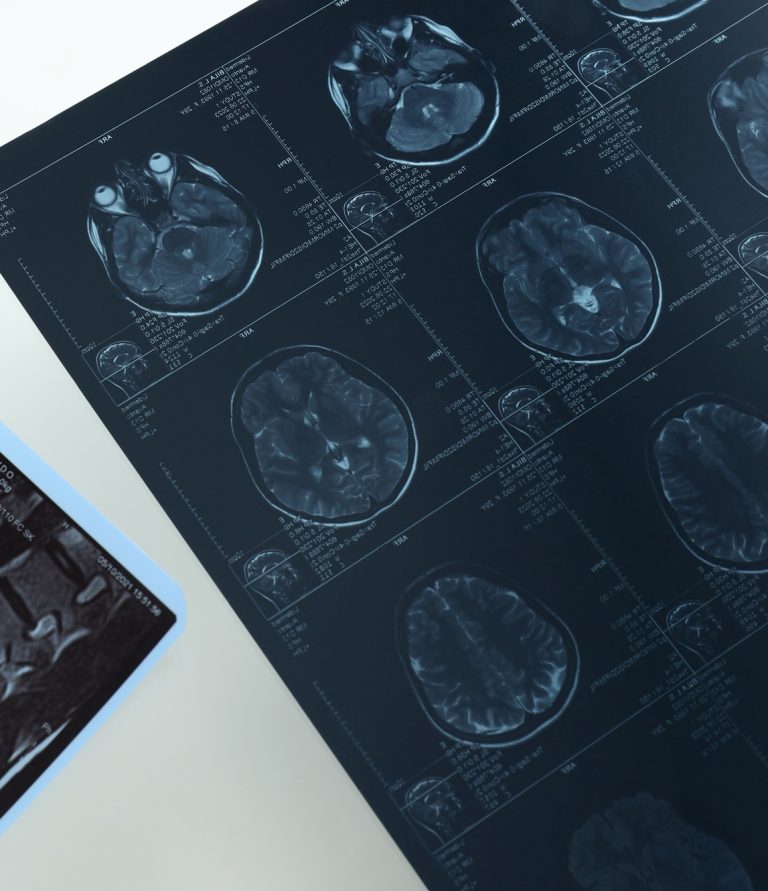
For patients with severe or long-standing hypertension, brain MRI is a valuable tool for detecting neurological complications. Chronic high blood pressure can lead to silent strokes—small, unnoticed brain infarcts that contribute to vascular dementia and cognitive decline. Brain MRI also helps identify white matter hyperintensities (WMH), which are associated with small vessel disease, a common consequence of long-term hypertension. In extreme cases, hypertensive crises can result in brain swelling (hypertensive encephalopathy) or intracerebral hemorrhage, both of which require immediate medical intervention. By identifying early signs of brain damage, imaging helps neurologists and cardiologists tailor treatment strategies to preserve cognitive function and reduce the risk of major strokes.
The integration of imaging into hypertension management allows for a comprehensive assessment of organ health, helping doctors personalize treatment plans and prevent life-threatening complications. Detecting early signs of heart strain, vascular disease, kidney dysfunction, or neurological damage enables timely interventions, including medication adjustments and lifestyle modifications. Regular monitoring, combined with non-invasive imaging techniques, plays a pivotal role in reducing hypertension-related morbidity and mortality. Ultimately, a combination of routine blood pressure checks, imaging assessments, and proactive management strategies remains the key to controlling hypertension and maintaining long-term cardiovascular health.